Noise Control in Healthcare Settings: Enhancing Patient Recovery
Hospitals are designed to restore health, yet the reality inside many facilities tells a different story. Beeping monitors, constant staff activity, HVAC systems, and corridor conversations often create soundscapes that are far from restful. Instead of promoting recovery, these environments expose patients to noise levels that exceed international health guidelines.
Research has shown that excessive hospital noise is linked to elevated stress levels, disturbed sleep cycles, and even longer recovery times. Studies indicate that when noise is reduced, patients heal faster, require fewer medications, and report higher satisfaction with their care environment.
Why Noise Control Matters in Healthcare
The modern hospital soundscape exposes patients to a constant mix of alarms, staff conversations, intercoms, trolleys moving through corridors, and mechanical systems such as HVAC units. This creates an acoustic environment that is far from therapeutic.
Excessive noise is not harmless. Clinical studies show that high noise levels in hospitals interfere with sleep, elevate stress hormones such as cortisol, and can even trigger cardiovascular strain in vulnerable patients. Poor sleep quality has a direct impact on the immune system, wound healing, and overall recovery time, making noise management a fundamental part of patient care.
The World Health Organisation has set clear benchmarks for hospital noise. Recommended levels are no more than 35 dB at night and 40 dB during the day. In reality, many hospital wards exceed these limits by significant margins, often averaging 55–70 dB. This discrepancy underscores the pressing need for improved acoustic planning and soundproofing strategies in healthcare facilities.

The Science Linking Noise and Patient Recovery
Noise in healthcare environments affects patients on multiple levels. Beyond being disruptive, it actively interferes with the biological and psychological processes essential for healing.
Sleep Architecture Disruption
Sleep is a cycle of light, deep, and REM phases. Each phase contributes to physical restoration, memory consolidation, and immune system regulation. In noisy wards, sleep becomes fragmented. Alarms, corridor activity, and equipment cycles often jolt patients awake, preventing them from reaching the deeper, restorative stages of sleep.
Consequences of disrupted sleep include:
- Slower tissue repair and wound healing
- Suppressed immune responses
- Increased fatigue, which delays rehabilitation and recovery
Psychological Effects
A noisy environment also weighs heavily on patients’ mental health. Continuous exposure to unpredictable sounds elevates stress levels and reduces the sense of safety needed in a healing space. Patients commonly report:
- Heightened anxiety and irritability
- Feelings of loss of control
- Reduced satisfaction with their hospital stay
In some cases, the perception of noise is as damaging as the volume itself. Even moderate noise, if irregular or unexpected, can cause more distress than steady background sounds.
Physical Outcomes
The physiological effects of noise have been documented in both short- and long-term recovery. Elevated stress hormones such as cortisol and adrenaline increase heart rate and blood pressure. Over time, this leads to strain on the cardiovascular system.
Evidence shows that:
- Patients in quieter wards often have shorter hospital stays
- High noise exposure correlates with higher reliance on sedatives and pain medication
- Wound healing slows when patients experience chronic sleep disruption and stress
By understanding these connections, healthcare providers can see that noise control is a matter of clinical significance with measurable effects on patient outcomes.

Common Noise Sources in Healthcare Facilities
Hospitals are dynamic environments, and their acoustic challenges vary depending on the space and its function. Identifying the main noise sources is the first step toward designing effective control strategies.
Patient Rooms
Patient rooms are intended to be restful spaces, yet they are often some of the noisiest areas in a hospital. Staff conversations in hallways, the movement of trolleys and equipment, and routine medical procedures introduce constant background noise.
Medical devices such as IV pumps and monitoring systems add repetitive sounds that patients cannot control. This continuous exposure disturbs sleep and increases stress levels and dissatisfaction with care.
Operating Theatres and ICUs
Critical care areas such as operating theatres and intensive care units are filled with life-saving equipment, but they also generate persistent noise.
Alarms from ventilators, infusion pumps, and monitors create an environment of constant alertness. Studies have shown that ICU noise levels regularly exceed WHO guidelines, averaging between 50 and 70 dB.
For patients who are sedated or critically ill, this can disrupt recovery and even slow weaning from mechanical ventilation. Staff performance may also be affected by alarm fatigue and difficulty concentrating in such a demanding environment.
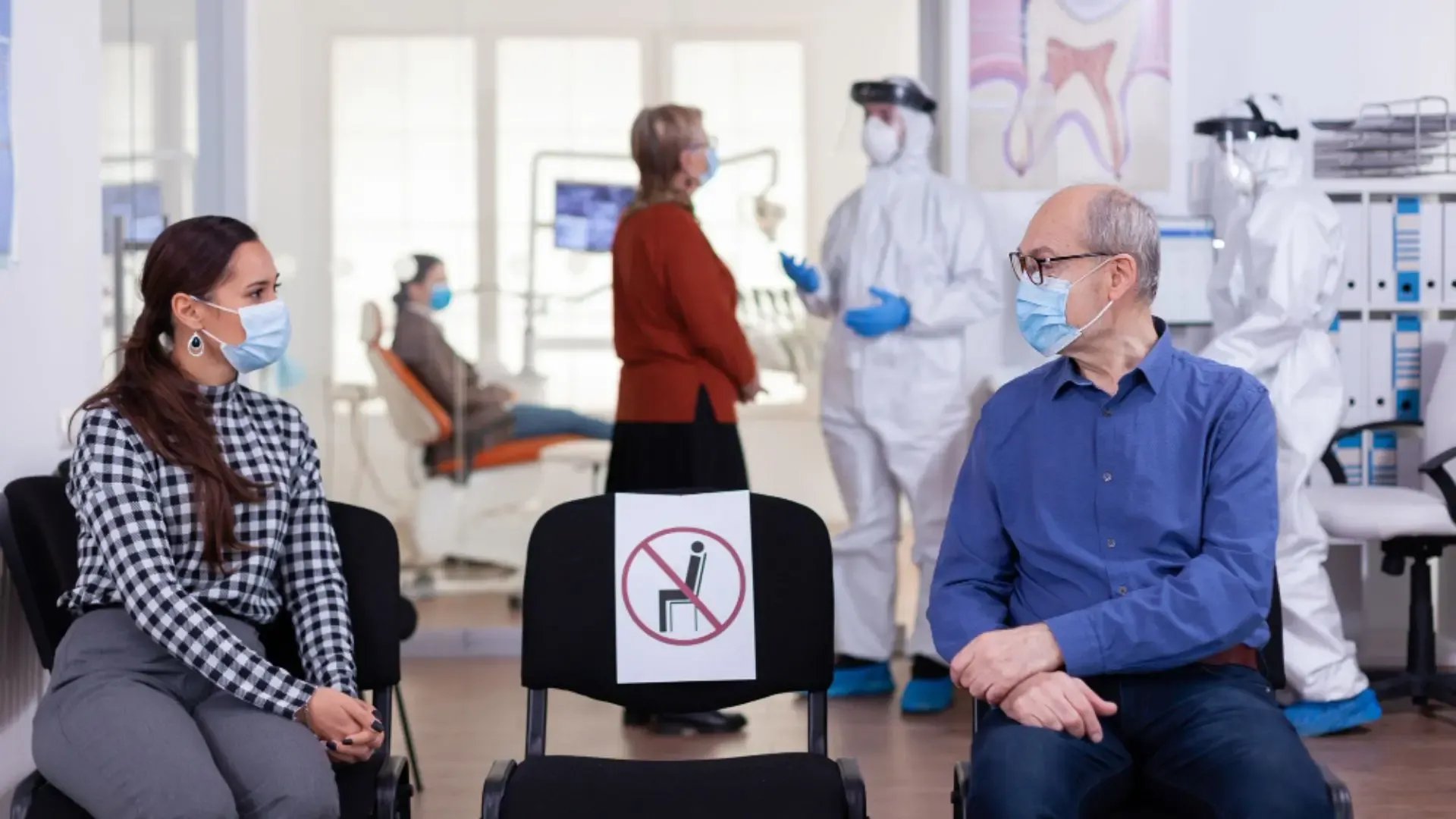
Waiting Areas and Diagnostic Zones
Noise challenges are not limited to treatment rooms. Waiting areas and diagnostic spaces experience high levels of foot traffic, conversations, and administrative activity.
Hard surfaces such as tiles, glass, and concrete cause sound to reverberate, amplifying the overall noise. In diagnostic areas such as imaging suites or audiology rooms, uncontrolled reverberation can interfere with communication between staff and patients, as well as the accuracy of certain tests.
Creating calmer, acoustically balanced spaces in these zones supports both patient comfort and operational efficiency.

Strategies for Effective Noise Control in Hospitals
Noise reduction in healthcare settings requires a multi-layered approach. Architectural planning, engineering solutions, and operational policies all contribute to creating quieter environments that support patient recovery.
Architectural Design Considerations
The foundation of hospital noise control begins at the architectural level. When acoustics are integrated into design from the outset, facilities face fewer disruptions, achieve higher patient satisfaction, and avoid costly retrofits later on. Architecture shapes how sound travels, reflects, and penetrates different spaces, which is why noise management must be considered alongside function and workflow.
- Layout and zoning play a critical role. By placing noisy areas such as nurses’ stations, supply rooms, and corridors away from patient recovery zones, hospitals can significantly reduce sound transfer into resting spaces. Creating buffer zones, for example, storage or utility rooms between high-traffic corridors and patient rooms, helps absorb and deflect noise.
- Absorptive materials are equally important. Hard, reflective surfaces like glass, ceramic tiles, and polished concrete may be easy to clean, but they create reverberation that amplifies every sound. Introducing sound-absorbing ceilings, acoustic wall treatments, and flooring materials with dampening qualities reduces this echo effect. In large open spaces such as waiting rooms or cafeterias, absorptive finishes can lower overall noise by several decibels, transforming the atmosphere into one more conducive to healing.
- Room orientation also contributes to acoustic performance. Locating recovery rooms, intensive care units, and consultation spaces away from mechanical plant rooms, elevators, or high-traffic entrances prevents exposure to constant low-frequency noise. Even within a ward, arranging beds so that headboards face internal rather than external walls can reduce disturbances from adjacent spaces.
By embedding acoustic thinking into floor plans and material choices, healthcare facilities create environments where patient rest, staff concentration, and medical accuracy are supported from the ground up. Architectural decisions that prioritise sound control deliver benefits that extend across the building’s entire lifecycle.
Engineering Solutions
Specialist engineering interventions are essential for reducing noise in healthcare environments, particularly in existing facilities where architectural modifications are limited. These interventions address both airborne noise, which travels through the air, and structure-borne noise, which moves through walls, floors, and ceilings. By combining different engineering strategies, hospitals can create acoustic environments that are safe, compliant, and patient-friendly.
Soundproof partitions and enclosures act as physical barriers to noise. They are especially effective in isolating loud equipment such as MRI scanners, HVAC plant rooms, or pump stations. High-density partitions built with layered composites prevent airborne noise from entering patient areas, while custom-built enclosures around machinery contain sound at the source. In surgical settings or intensive care units, mobile acoustic partitions can also be used as flexible solutions to create quieter micro-environments.
Acoustic panels enhance acoustic clarity by reducing reverberation and echo. In large spaces such as waiting areas, wards, or diagnostic zones, panels absorb sound energy that would otherwise bounce off reflective surfaces. By lowering reverberation times, panels improve speech intelligibility between staff and patients, which is critical in healthcare environments where clear communication affects both comfort and safety. Panels can be ceiling-mounted, wall-mounted, or integrated into modular room dividers, offering design flexibility that blends with the hospital’s aesthetics.
Damping materials and vibration control systems target structure-borne sound. Vibrations from HVAC units, lifts, pumps, or mechanical beds often travel through building frames and re-radiate as noise in sensitive rooms. Isolation pads, resilient mounts, and spring systems break this transmission path, reducing the transfer of low-frequency vibration into recovery areas. In operating theatres or imaging suites, vibration control is particularly important to protect both patients and sensitive diagnostic equipment.
These engineered measures are not one-size-fits-all. Each department has its own acoustic profile, shaped by equipment type, room geometry, and patient needs. For example, a neonatal intensive care unit demands extremely low noise thresholds to protect vulnerable infants, whereas a diagnostic imaging suite requires both vibration isolation and absorption to preserve test accuracy. Tailoring solutions to these specific conditions ensures compliance with WHO and national noise standards while supporting hospital functionality and patient well-being.
Operational Policies
Even the best materials cannot control noise without appropriate management practices. Hospitals benefit from operational policies that reduce unnecessary disturbances:
- Staff training on the importance of quiet care and communication practices
- Quiet hours to protect patient sleep cycles, especially during night shifts
- Routine equipment maintenance to prevent alarms, squeaks, and hums from escalating
- Behavioural adjustments such as closing doors gently, lowering voices in corridors, and reducing alarm volume when safe
Operational policies build a culture of awareness where every member of staff plays a role in sustaining an acoustically calm environment.
Creating Healing Environments Through Acoustic Design
Noise control is a core factor in patient recovery, satisfaction, and clinical excellence. A well-managed acoustic environment supports restful sleep, lowers stress, and helps staff deliver safer and more focused care. By addressing both the architectural and operational dimensions of hospital noise, healthcare facilities can transform their spaces into true healing environments.
DECIBEL brings together engineering precision and human-centred design to deliver noise control solutions tailored to the demands of modern healthcare. From acoustic modelling to the installation of soundproof partitions, panels, and vibration control systems, our expertise ensures compliance with standards while prioritising patient comfort.
Get in touch with our team today to discuss a consultation or design assessment for your healthcare facility and create a quieter, restorative space for patients and staff.



